Part 6: Resuscitation Education Science
- Effective education is an essential contributor to improved survival outcomes from cardiac arrest.
- Use of a deliberate practice and mastery learning model during resuscitation training improves skill acquisition and retention for many critical tasks.
- The addition of booster training to resuscitation courses is associated with improved cardiopulmonary resuscitation (CPR) skill retention over time and improved neonatal outcomes.
- Implementation of a spaced-learning approach for resuscitation training improves clinical performance and technical skills compared with massed learning.
- The use of CPR feedback devices during resuscitation training promotes CPR skill acquisition and retention.
- Teamwork and leadership training, high-fidelity manikins, in situ training, gamified learning, and virtual reality represent opportunities to enhance resuscitation training and may improve learning outcomes.
- Self-directed CPR training represents a reasonable alternative to instructor-led CPR training for lay rescuers.
- Middle school– and high school–age children should be taught how to perform high-quality CPR because this helps build the future cadre of trained community-based lay rescuers.
- To increase bystander CPR rates, CPR training should be tailored to low–socioeconomic status neighborhoods and specific racial and ethnic communities, where there is currently a paucity of training opportunities.
- Future resuscitation education research should include outcomes of clinical relevance, establish links between performance outcomes in training and patient outcomes, describe cost-effectiveness of interventions, and explore how instructional design can be tailored to specific skills.
Each year, millions of providers receive basic and advanced life support training with the aim of improving patient outcomes from cardiac arrest.1 Resuscitation training programs incorporate evidence-based content while providing opportunities for learners to practice lifesaving skills in individual and team-based clinical environments. While resuscitation training is widespread, learners frequently fall short of achieving the desired performance outcomes, resulting in skills that do not consistently translate to clinical care with real patients.1,2
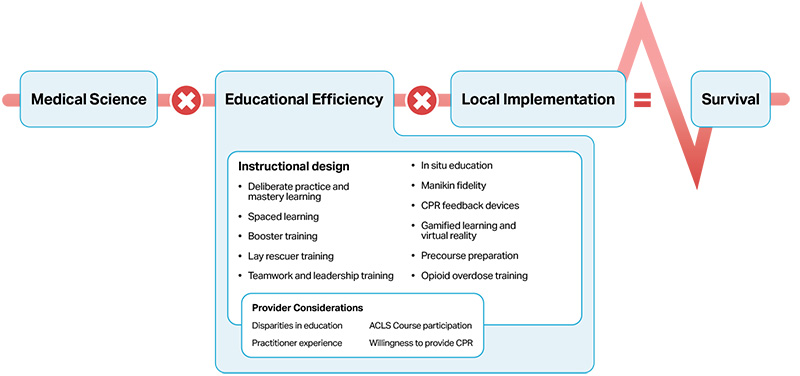
The International Liaison Committee on Resuscitation Formula for Survival (Figure 1.) emphasizes 3 essential components influencing survival outcomes from cardiac arrest: guidelines based on current resuscitation science, effective education of resuscitation providers, and local implementation of guidelines during patient care.3 Greater emphasis on effective education will improve provider performance, enhance local implementation of guidelines, and potentially increase survival rates from cardiac arrest.
Cardiac arrest remains a major public health problem, with more than 600 000 cardiac arrests per year in the United States.1,2 Survival rates of patients with cardiac arrest remain low despite advancements in resuscitation science.3 Each year, millions of people receive basic and advanced life support training in an effort to improve the quality of care delivered to cardiac arrest patients.4 Resuscitation training programs are designed to convey evidence-based content and provide opportunities for learners (ie, those enrolled in resuscitation training programs) to apply knowledge and practice critical skills. These programs, however, frequently fall short of achieving the desired learning outcomes (eg, knowledge and skill acquisition), with performance that does not consistently translate over to the real-world clinical environment.4,5 For example, cardiopulmonary resuscitation (CPR) skills that are acquired immediately after basic life support (BLS) training often show decay by as early as 3 months, resulting in many BLS-trained healthcare providers—such as physicians, nurses, respiratory therapists, and other healthcare professionals— struggling to perform guideline-compliant CPR during simulated and real cardiac arrests.6–14 Additionally, current research on lay rescuer CPR training is lacking evidence describing the optimal methods to train bystanders to recognize cardiac arrest, initiate CPR, and use automated external defibrillators appropriately.15–17 A dedicated focus on instructional design is essential to ensure that knowledge and skills acquired during training are applied when caring for patients in cardiac arrest.4
Improving survival from cardiac arrest is highly dependent on the quality of resuscitative care. Many key determinants of survival, such as immediate recognition of cardiac arrest, early initiation of CPR, early defibrillation, and high-quality chest compressions, are variables that can be targeted by resuscitation training programs to improve patient outcomes. Instructional design features are the key elements, or “active ingredients,” of resuscitation training programs that determine how content is delivered to the learner.18A better understanding of the impact of instructional design features on learning outcomes will enable educators to design training programs that translate into outstanding clinical performance during cardiac arrests. Furthermore, appreciating how social determinants of health (eg, SES, race) and individual factors (eg, practitioner experience) influence the downstream impact of resuscitation education will help inform future policy and implementation strategies. In this Part, we describe the evidence supporting key elements of resuscitation education and provide recommendations aimed at improving learner outcomes and patient outcomes from cardiac arrest.
The following sections briefly describe the process of evidence review and guideline development. See “Part 2: Evidence Evaluation and Guidelines Development” in the 2020 ECC Guidelines for more details on this process.19
The Resuscitation Education Science Writing Group comprised a diverse team of experts with backgrounds in resuscitation education, clinical medicine (ie, pediatrics, intensive care, emergency medicine), nursing, prehospital care, health services, and education research. Writing group members are American Heart Association (AHA) volunteers with an interest and recognized expertise in resuscitation and are selected by the AHA Emergency Cardiovascular Care (ECC) Committee. The AHA has rigorous conflict-of-interest policies and procedures to minimize the risk of bias and improper influence during development of the guidelines.20 Before appointment, writing group members and peer reviewers disclosed all commercial relationships and other potential (including intellectual) conflicts. Comprehensive disclosure information for writing group members is listed in Appendix 1.
This Part of the 2020 AHA Guidelines for CPR and ECC is based on the extensive evidence evaluation performed in conjunction with the International Liaison Committee on Resuscitation and affiliated International Liaison Committee on Resuscitation member councils. Three different types of evidence reviews (systematic reviews, scoping reviews, and evidence updates) were used in the 2020 process. Each of these resulted in a description of the literature that facilitated guideline development.21–25 Reviews were limited to the resuscitation education science literature, but many of the concepts reviewed have origins within other fields (eg, medical education, psychology).
The AHA Resuscitation Education Science Writing Group reviewed all relevant and current AHA Guidelines for CPR and ECC5,26–37and the relevant 2020 International Consensus on CPR and ECC Science With Treatment Recommendations27 to determine if current guidelines should be reaffirmed, revised, or retired and whether new recommendations were needed. The writing group then drafted, reviewed, and approved recommendations (by majority vote among members), assigning to each a Level of Evidence (LOE; ie, quality) and Class of Recommendation (COR; ie, strength; see Table 1. Applying COR and LOE to Clinical Strategies, Interventions, Treatments, or Diagnostic Testing in Patient Care).
Importantly, applying Grading of Recommendations, Assessment, Development, and Evaluation (GRADE)38 to educational studies yields greater challenges than its application to clinical studies. Specific considerations for studies involving educational outcomes (eg, improved “outcomes” in simulated patient settings or improved performance on summative assessment tools) are not provided in GRADE methodology; the writing group frequently assigned LOE to these studies according to a combination of a typical review of study quality, perceived importance of underlying constructs in the context of educational science, and (where possible) extrapolation of findings to analogous clinical phenomena (eg, outcomes in real patients as opposed to simulated ones).
The 2020 guidelines are organized into knowledge chunks, grouped into discrete modules of information on specific topics or management issues.39 Each modular knowledge chunk includes a table of recommendations using standard AHA nomenclature of COR and LOE. A brief introduction or short synopsis puts the recommendations into context with important background information and overarching management or treatment concepts. Recommendation-specific supportive text clarifies the rationale and key study data supporting the recommendations. Hyperlinked references are provided to facilitate quick access and review.
These guidelines were submitted for blinded peer review to subject matter experts nominated by the AHA. Peer reviewer feedback was provided for guidelines in draft format and again in final format. The guidelines were reviewed and approved for publication by the AHA Science Advisory and Coordinating Committee and the AHA Executive Committee. Comprehensive disclosure information for peer reviewers is listed in Appendix 2.
| Abbreviation | Meaning/Phrase |
|---|---|
| ACLS | advanced cardiovascular life support |
| AHA | American Heart Association |
| B-CPR | bystander cardiopulmonary resuscitation |
| BLS | basic life support |
| COR | Class of Recommendation |
| CPR | cardiopulmonary resuscitation |
| ECC | emergency cardiovascular care |
| EMS | emergency medical services |
| EO | expert opinion |
| LD | limited data |
| LOE | Level of Evidence |
| NR | nonrandomized |
| OHCA | out-of-hospital cardiac arrest |
| PALS | pediatric advanced life support |
| RCT | randomized controlled trial |
| ROSC | return of spontaneous circulation |
| SES | socioeconomic status |
| VR | virtual reality |
Open table in a new window
In 2018, the AHA published a scientific statement, titled “Resuscitation Education Science: Educational Strategies to Improve Outcomes From Cardiac Arrest,”1 providing a comprehensive synthesis of the evidence supporting best educational practices for resuscitation. The topics explored in the statement were framed by the Formula for Survival in Resuscitation (Figure),2 which describes the contributions of medical science (ie, guideline quality), educational efficiency (ie, quality and impact of education), and local implementation (ie, uptake and adoption of guidelines) toward improving survival outcomes from cardiac arrest. These guidelines complement the scientific statement by providing an updated review of the science and highlighting specific recommendations to support evidence-informed change in resuscitation education.
These guidelines comprise 3 main sections: instructional design, provider considerations, and knowledge gaps and future research. Resuscitation training programs may incorporate 1 key instructional design feature, or they may be blended in an effort to optimize learning outcomes. The best instructional designs are tailored to specific learning objectives, learner type, and context of learning. Here, we offer recommendations related to the use of deliberate practice and mastery learning, booster training and spaced learning, lay rescuer training, teamwork and leadership training, in situ education, manikin fidelity, CPR feedback devices in training, gamified learning and virtual reality (VR), precourse preparation for advanced courses, and special considerations for training in the management of opioid overdose. As highlighted in the Figure, instructional design features contribute to educational efficiency in the Formula for Survival.
In the second section, we describe how certain provider considerations may influence the overall impact of education. For example, disparities in access to resuscitation education (eg, SES, race) or prior provider experience may contribute positively or negatively to learning outcomes. Some providers may decide to take the AHA Advanced Cardiovascular Life Support (ACLS) Course, whereas others may not. How does this influence patient outcomes? All of these considerations feed into the potential impact of instructional design and ultimately influence the educational efficiency component of the Formula for Survival (Figure).
In reviewing content for these guidelines, the writing group identified and discussed many important topics relevant to resuscitation education, such as the role of cognitive load in learning, the use of augmented reality, blogs and podcasts as educational tools, learner assessment, training in low-resource settings, and the role of faculty development for training resuscitation educators. While these and other topics represent areas of interest, there was insufficient evidence examining the impact of these concepts on resuscitation education to support the development of recommendations. We refer interested readers to the AHA scientific statement “Resuscitation Education Science: Educational Strategies to Improve Outcomes From Cardiac Arrest” for a discussion of these concepts.1 More literature is required before these issues can be incorporated into future iterations of the AHA Guidelines. We conclude this Part of the 2020 Guidelines with a summary of current knowledge gaps in resuscitation education science and a discussion of future directions for optimizing the impact of resuscitation training programs.
| COR | LOE | Recommendation |
|---|---|---|
| 2b | B-NR |
|
Synopsis
Deliberate practice is a training approach where learners are given (1) a discrete goal to achieve, (2) immediate feedback on their performance, and (3) ample time for repetition to improve performance.13,14 Mastery learning is defined as the use of deliberate practice training along with testing that uses a set of criteria to define a specific passing standard that implies mastery of the tasks being learned.15 A better understanding of how deliberate practice and mastery learning can be implemented in resuscitation training would help enhance training and patient outcomes. Twelve studies have examined the impact of deliberate practice and/or mastery learning in resuscitation training.1–12 Eight studies demonstrated improved learner performance with deliberate practice and mastery learning (eg, scores on clinical assessments, time to interventions)1,2,5–10 whereas other studies found no difference in learner outcomes.3,4,11,12 Because the majority of studies report positive results, we recommend that deliberate practice and mastery learning be incorporated into basic and advanced life support training. Specifically, we recommend pairing repetition with customized feedback that is based on assessments, assigning specific exercises to address weaknesses, and providing learners sufficient time to attain the minimum passing standard for a specific skill. Future research should use consistent definitions for deliberate practice and mastery learning and seek to isolate the effect of deliberate practice and mastery learning through the use of appropriate and clearly defined comparator groups.
Recommendation-Specific Supportive Text
- Two of 4 randomized controlled trials (RCTs) found that learners exposed to deliberate practice demonstrated improved clinical performance and decreased time to perform critical interventions (eg, time to ventilation, time to epinephrine) on simulated patients.1,2 Two of 4 RCTs found no significant difference in learner outcomes with deliberate practice compared with traditional training.3,4
Six of the 8 observational studies found an association between deliberate practice and mastery learning and improved performance measures in simulated patients (eg, time to compression, time to defibrillation, checklist scores).5–10 Two studies involving lay rescuers (1 RCT and 1 observational) showed no improved performance associated with deliberate practice and mastery learning.4,11 Skill decay was measured in 5 studies.5,9–12 Four studies found no significant decay after deliberate practice and mastery learning for up to 6 months,9–12 and 1 study found a significant linear decline (P=0.039) in performance at 6 months after training.5 In one study, onetime costs associated with incorporating a deliberate practice and mastery learning model into resuscitation training were higher than for traditional training, whereas recurring costs were lower because of decreased instructor involvement.12 Future studies should explore if deliberate practice and mastery learning are less costly over time for training larger groups of learners.
Most current resuscitation courses use a massed learning approach: a single training event lasting hours or days, with retraining every 1 to 2 years.1 Other resuscitation courses use a spaced learning approach, involving the separation of training into multiple sessions, each lasting minutes to hours, with intervals of weeks to months between sessions.2–5 Each spaced session involves the presentation of new content and/or the repetition of content from prior sessions. Booster training is another instructional design feature, involving brief weekly or monthly sessions focused on repetition of content presented in an initial massed learning course.6–18
Frequent booster trainings (at intervals of 1–6 months) were associated with improved CPR skills.6–9,14,16,18 Reduced mortality was noted after implementation of weekly boosters for neonatal training.13 One study reported that learners were less likely to attend all sessions with increased frequency of boosters, with the highest learner attrition in the group practicing every month.6 No studies evaluated booster training for pediatric advanced life support (PALS) or ACLS courses. Spaced learning courses are of equal or greater effectiveness than massed learning courses for pediatric resuscitation training.3–5 No studies compared spaced learning with massed learning for BLS, neonatal (eg, Neonatal Resuscitation Program), or ACLS courses. We recommend that resuscitation training programs implement boosters when a massed learning approach is used and consider implementing spaced learning courses in place of massed learning. Future research is needed to determine optimal training intervals while concurrently minimizing costs and ensuring learner engagement over time.
| COR | LOE | Recommendation |
|---|---|---|
| 1 | B-R |
|
Recommendation-Specific Supportive Text
- Seven RCTs compared booster CPR training, at intervals of 1 to 6 months, with no booster training and found improvements in CPR performance.6–9,14,16,18 In 1 RCT, nurses randomized to more frequent CPR booster training demonstrated dose-dependent improvement in CPR skills at 1 year (proportion with overall excellent CPR at 12 months: 58% every 1 month boosters, 26% every 3 months, 21% every 6 months, 15% every 12 months).6 The monthly group, however, was least likely to complete all sessions. In a second RCT, emergency department providers randomized to monthly CPR booster training demonstrated a higher percentage of providers who could perform excellent CPR at 12 months compared with those who received no boosters (excellent CPR on adult manikin: 54.3% versus 14.6%; P<0.001; infant manikin: 71.7% versus 19.5%; P<0.001).14 Additional RCTs demonstrated improvements in knowledge and CPR skills after 30-minute boosters at 1, 3, and 6 months7 ; enhanced ventilations and compressions after 6-minute monthly boosters8,16; and shorter time to start compression and defibrillation after 15-minute boosters every 2, 3, or 6 months.18
Three RCTs reported that more frequent Neonatal Resuscitation Program boosters (ie, weekly to every 9 months) were associated with improved skill performance over time,10–12 and 1 observational study described improved clinical performance and reduced infant mortality (pre: 11.1/1000 versus post: 7.2/1000; P=0.04) after 3- to 5-minute weekly boosters.13
| COR | LOE | Recommendation |
|---|---|---|
| 2a | B-R |
|
Recommendation-Specific Supportive Text
- Two RCTs and 1 observational study compared spaced learning with massed learning for pediatric resuscitation training.3–5 In 1 RCT, emergency medical services (EMS) providers were randomized to either spaced learning (four 3.5-hour weekly sessions) or massed learning (2 sequential 7-hour days).3 Compared with the massed learning group, the spaced learning group had superior retention of infant bag-mask ventilation and infant intraosseous insertion skills at 3 months but no difference in chest compression skills. Knowledge decay was noted in the massed learning group but not in the spaced learning group.3
In another RCT, pediatric nurses and respiratory therapists were randomized to either spaced learning (six 30-minute sessions over 6 months) or massed learning (one 7.5-hour day) for PALS recertification.5 Clinical performance scores improved in the spaced learning group. Both groups demonstrated similar improvements in teamwork measured at course completion.
In an observational study, medical students completed either spaced learning (four 1.25-hour weekly sessions) or massed learning (one 5-hour session) for pediatric resuscitation skills. No difference was noted in knowledge or global ratings of skills (ie, bag-mask ventilation, intraosseous insertion, or chest compression) measured at 4 weeks after course completion between the groups.4
| COR | LOE | Recommendations |
|---|---|---|
| 1 | C-LD |
|
| 1 | C-LD |
|
| 2a | C-LD |
|
| 2a | C-LD |
|
| 2a | A |
|
| 2b | B-R |
|
| 2b | C-LD |
Synopsis
Immediate CPR can double or triple survival rates after cardiac arrest.58,59 The primary goal of resuscitation training for lay rescuers (ie, non–healthcare professionals) is to increase immediate bystander CPR (B-CPR) rates, automated external defibrillator use, and timely emergency response system activation during an OHCA. Enhancing willingness to perform CPR in this population may have a direct impact on survival rates for OHCA.60 This modular knowledge chunk looks at the question, Among lay rescuers, what features of CPR training and/or the context of training affect willingness to perform CPR in actual resuscitations, skill-performance quality, and patient outcomes?
The evidence reviewed suggests that lay rescuers should attend an instructor-led and/or self-directed CPR training session with real-time or delayed feedback to improve CPR skills.1–4 Training sessions should use combinations of skill-specific training strategies designed to enhance CPR skill retention.54–57 Refresher training, which focuses on skills and self-confidence rather than on knowledge, should be undertaken regularly, although the optimal time frame requires further study.4,53–57 It is reasonable for communities to train lay rescuers in compression-only CPR rather than in traditional ventilation-and-compression CPR.19,20 High-quality CPR is associated with improved survival; however, there are no studies to date that directly correlate CPR performance assessed on a manikin with real patient outcomes.
Recommendation-Specific Supportive Text
- Four studies examined self-instruction without instructor involvement versus an instructor-led course and showed no significant difference.1–4 Brief video instruction has shown improved compression rates compared with no training 5,6 ; however, instructor-led training is slightly superior in improving compression depth and hand placement and minimizing interruptions.6–9
- Multiple studies have found that middle school– and high school–age children are capable of learning and recalling high-quality CPR skills.10–18 Early training in middle school and high school may instill confidence and a positive attitude toward responding in a real-life situation.
- Studies have found that, compared with conventional CPR programs, compression-only CPR programs result in a greater number of appropriate chest compressions by lay rescuer learners.19,20 When surveyed, lay rescuers report a greater willingness to provide compression-only CPR than they do for conventional CPR with assisted ventilations.21–23 Two studies published after a statewide educational campaign for lay rescuers showed that the prevalence of both overall B-CPR and compression-only CPR increased over time, but no effect on patient survival was demonstrated.24,25
- Many studies have looked at the effectiveness of BLS training in family members and/or caregivers of high-risk cardiac patients. Outcomes included frequency at which CPR is performed by family members; knowledge, skills, and adequacy of performance; and the survival rates of cardiac arrest victims receiving CPR from family members. The majority of trained lay rescuers were able to competently perform BLS skills, reported a willingness to use these skills, and experienced lower anxiety.26–39 More research is required to demonstrate a clear benefit because many studies reported low numbers of OHCA and high loss of follow-up.
- Lay rescuers who used devices that provided corrective feedback during CPR training had improved compression rate, depth, and recoil compared with learners performing CPR without feedback devices.40–44 Evidence of the effect of feedback devices on CPR skill retention is limited, with 1 of 4 studies demonstrating improved retention.41,45–47
- Three randomized trials examined the use of auditory guidance (ie, use of a metronome or music) to guide CPR performance during lay rescuer training.48–50 All found that chest compression rate was improved when auditory guidance was used, although 1 study reported a negative impact on chest compression depth. Training with guidance from a popular song has been shown to prevent deterioration of chest compression rate over time.48,51,52
- Studies have demonstrated the deterioration of CPR skills of lay rescuers in as little as 3 months after initial training.4,53 Shorter and more frequent training sessions have demonstrated slight improvement in knowledge and chest compression performance and shorter time to defibrillation.54–57
| COR | LOE | Recommendation |
|---|---|---|
| 2a | B-NR |
|
Synopsis
Resuscitation of cardiac arrest patients relies on multiple providers working together to coordinate delivery of time-sensitive therapies, making teamwork and leadership indispensable components of providing optimal care.16–18 Training that focuses on the communication and interpersonal skills required for teams to work as a coordinated unit can have a potential impact on patient outcomes.19–21 Studies evaluating the effect of team and leadership training when included as part of advanced life support training for healthcare providers have found a positive impact on provider skills during simulated and real cardiac arrests.1–15,22 These studies included a broad range of educational strategies (eg, video modules, simulation) and outcome measures (eg, quality of communication, adherence to recommended advanced life support practices). Despite the low-moderate quality of evidence, we recommend including team and leadership training as part of advanced life support training for healthcare providers. This recommendation is justified because the potential benefit from team and leadership training significantly outweighs the potential risks. Further studies are needed to define the optimal educational strategies for team and leadership training as well as to understand the interplay and relative benefit among team, leadership, and skills training on provider skill and patient outcomes.
Recommendation-Specific Supportive Text
- Several studies examined the impact of team or leadership training on patient outcomes or provider skills in actual cardiac arrests. One prospective observational study reported an increase in survival from pediatric cardiac arrests from 33% to approximately 50% (P=0.00) within 1 year of implementing a formal hospital-wide mock code team training program.1 One RCT of simulation-based leadership training found no effect on CPR quality during resuscitation of patients.6 Four observational studies found an association between interventions to improve teamwork and CPR quality, communication, and deployment times for mechanical devices.2–5
Seven RCTs and 1 multicenter prospective interventional study explored the impact of team and leadership training on performance of clinical tasks in simulated resuscitations, both at course completion and at follow-up from 3 to 15 months later.7–14 Each of the studies showed improvement in 1 or more aspects of performance, although improvements were not universal across all measures. Improvements were seen in both specific aspects of clinical care, such as time to initiation of CPR and time to defibrillation,7–13 and compliance with ACLS guidelines.12–14 Ten RCTs reported that team or leadership training was associated with improvement in measures of teamwork and leadership during simulated resuscitations, such as frequency of leader vocalizations,8,10,14 frequency of specific team skills,7,11,13,23 and scores on various teamwork rating scales.9,11,12,15
| COR | LOE | Recommendations |
|---|---|---|
| 2a | C-LD |
|
| 2b | B-R |
|
Synopsis
In situ simulation refers to a subset of simulation activities occurring in actual patient care areas (ie, real clinical environment).16 In situ simulation can be used as a strategy to train individuals and/or healthcare teams.17,18 The objectives for in situ training can be individual provider technical skills or team-based skills, including communication, leadership, role allocation, and situational awareness.17,18 One distinct advantage of in situ training is that it provides learners with a more realistic training environment. In this review, we explored if in situ, simulation-based resuscitation training for healthcare providers leads to improved learning, performance, and/or patient outcomes.
Studies comparing in situ training to traditional training (ie, classroom or laboratory-based training) have not demonstrated significant differences in learning outcomes.13–15 Compared with no intervention, in situ training added to other educational strategies has a positive impact on learning outcomes (eg, improved team performance, improved time to critical tasks),2,7–12 performance change in the real clinical environment (eg, improved team performance, recognition of deteriorating patients),2–4 and patient outcomes (eg, improved survival, neurological outcomes).1,4–6 The advantages of in situ training should be weighed against the potential risks, including logistical challenges of conducting training in clinical spaces and risks of mixing training resources with real clinical resources (eg, simulated versus real medications or fluids).19,20
Recommendation-Specific Supportive Text
- Three observational studies demonstrated that regular in situ simulation training, in combination with other educational strategies (ie, refresher of BLS/PALS training, introduction of code teams, distributed practice), is effective at improving team performance and time to recognize deteriorating patients.2–4 Four additional observational studies assessing bundled interventions including in situ training demonstrated significant improvements in cardiac arrest survival.1,4–6 Because in situ training was tested as part of a bundled intervention in these studies, the individual contribution of in situ training cannot be clearly elucidated.
Two RCTs demonstrated that in situ cardiac arrest training coupled with spaced learning yields better learning outcomes (ie, improved clinical performance, decreased time to initiate compression and defibrillation) compared with training conducted in a massed-delivery format in the classroom.8,9 One RCT and 4 prospective observational studies demonstrated that in situ simulation training results in improved clinical performance in simulated environments.2,7,10–12 Most observational studies are limited by a lack of parallel control groups, a lack of performance measures with supportive validity evidence, and potential confounding factors. - Two RCTs and 1 observational study compared learning outcomes (ie, team performance, technical skills) of in situ simulation training with standard classroom or laboratory-based training settings and demonstrated no significant differences between the 2 settings.13–15
| COR | LOE | Recommendations |
|---|---|---|
| 2a | B-R |
|
| 2b | C-LD | |
| 2b | C-EO |
Synopsis
Learner engagement during resuscitation education is enhanced by optimizing the reality of the training experience.1 Three different categories of fidelity (or realism) have been described: (a) conceptual fidelity (ie, the concepts and relationships presented in the simulation); (b) emotional fidelity (ie, the holistic experience of the simulation); and (c) physical fidelity (ie, the properties of the manikin and the environment).7 Manikins are a full or partial body representation of a patient.8 The term manikin fidelity has been used to refer to the presence of simulated physical features that can be used to more closely mimic a resuscitation patient.2 Higher-fidelity manikins with advanced physical features allow simulation of patients across age groups (eg, newborn, infant, child, adult) and physiological states (eg, traumatic injury, pregnancy, cardiac arrest). Use of higher-fidelity manikins could theoretically improve learner immersion and engagement in scenario-based learning. Disadvantages of higher-fidelity manikins include increased costs to purchase, the need for trained personnel to operate them, and the need for ongoing maintenance.1
Studies examining the impact of higher-fidelity manikins during resuscitation education have yielded varied results. A recent systematic review found that using higher-fidelity manikins in resuscitation training led to improved skill acquisition at course completion but no impact on long-term skills or knowledge.2 For the current update, we identified 2 RCTs examining the impact of manikin fidelity on trainee knowledge and psychomotor skill, with mixed results.3,4 No studies assess the impact of manikin fidelity on patient outcomes. Using higher-fidelity manikins can be beneficial when availability and supportive infrastructure permit their use. This recommendation must be balanced against the cost and training requirements for manikin operators as well as the need for accurate alignment of manikin features with learning objectives.
Recommendation-Specific Supportive Text
- A meta-analysis of studies assessing the impact of higher-fidelity manikins during resuscitation education found a moderate benefit on skill performance at course conclusion but no impact on long-term skills or knowledge.2 The review acknowledged the increased cost and the need for trained personnel to operate higher-fidelity manikins. One nonrandomized trial of PALS training compared knowledge (examination score) and skill (task performance time) for intervention group trainees who used a higher-fidelity infant manikin with control group trainees who used a standard manikin. No differences were found in knowledge or skill at course completion, though knowledge at 6 months after course completion was higher in the higher-fidelity group.4
- An RCT of a neonatal resuscitation program training medical students compared knowledge (ie, examination score) and skill (ie, Megacode score) for intervention trainees who used a higher-fidelity manikin (ie, with observable vital signs, cyanosis, limb movements, and breath sounds) with control trainees who used a basic manikin without these features. No significant differences were found in skill or knowledge at course completion or at 3 months between the intervention and control groups.3
- Tailoring manikin selection (ie, physical features) to the needs of the scenario and the scope of trainees’ practice ensures that required physical features are present to maximize learner engagement.6
| COR | LOE | Recommendation |
|---|---|---|
| 2a | B-R |
|
Synopsis
Accurate assessment of CPR skills is critical to helping learners improve performance.11 Prior studies demonstrate that visual assessment of CPR quality is neither reliable nor accurate, making it challenging for instructors to provide consistently meaningful feedback during CPR training.12–15 Feedback devices address this problem by providing objective feedback to learners and instructors during practice. CPR feedback devices can be grouped into 2 categories: corrective feedback devices (eg, visual display of depth) and prompt devices that provide an auditory tone for the provider to follow (eg, metronome). In this review, we assessed if the use of CPR feedback devices during training, compared with no use of feedback devices during training, improves CPR skills, clinical performance, and patient outcomes.16
Studies examining the use of CPR feedback devices during training showed mixed results, with 6 of 8 studies demonstrating improved CPR skill performance at the conclusion of training.1–6,17,18 The use of corrective feedback devices during training resulted in improved skill retention at 7 days to 3 months after initial training compared with learners trained without a feedback device.2,6–10,19 No studies have reported the cost-effectiveness of feedback device use during training or the impact on healthcare providers’ performance in clinical settings and patient outcomes. The benefit of feedback use during training should be balanced with the cost of such devices as well as the potential increased cognitive processing for learners during CPR training.
Recommendation-Specific Supportive Text
- Seven RCTs and 1 observational study examined the use of feedback devices during training relative to no use of feedback devices during training or instructor-led training.1–6,17,18 Six studies demonstrated significant improvement in CPR skills at course completion when feedback devices were used during training,1–6 whereas 2 studies failed to demonstrate benefit with CPR feedback device use.17,18 Five RCTs and 2 observational studies demonstrated that feedback device use during training was associated with significantly improved CPR skill retention at 7 days to 3 months.2,6–10,19
Some studies used lay rescuers, junior trainees, or medical students as the study population, limiting the generalizability of the findings to practicing healthcare providers.2,3,5,9,10,17–19 Other studies combined real-time feedback with other educational strategies,6,19 making it difficult to isolate the true impact of feedback device use. Future research should consider linking CPR feedback device use during training with actual patient outcomes or clinical performance of healthcare providers and reporting the cost-effectiveness of feedback device use during training.
| 2b | B-R |
|
|---|---|---|
| 2b | B-NR |
|
Synopsis
Increasingly, the use of gamified learning and VR is being considered for training lay rescuers and healthcare providers.11,12 Gamified learning includes leaderboards and serious games. Leaderboards are used for the purpose of increasing the frequency of practice by incorporating competition among trainees, whereas serious games are designed specifically for use of play (ie, board games, computer-based games) around a “serious” topic, such as resuscitation.6,13 VR is a computer generated interface with which a user can interact in a three-dimensional world in which objects have a sense of spatial presence.14,15
Review of the gamified learning and VR literature demonstrated mixed results, with some studies showing improved knowledge acquisition, knowledge retention, and CPR skills with these learning modalities,1–5,7,16 whereas other studies showed no benefit.6,8–10,17,18 No studies demonstrated a negative impact on learning. The effect of gamified learning and VR on performance during real cardiac arrests or on patient outcomes is unknown. Incorporation of gamified learning and VR into resuscitation programs should consider start-up costs associated with purchasing equipment and relevant software. Augmented reality, which incorporates a computer-generated holographic image overlaid into the real environment, was not included in this review because of a lack of relevant research.
Recommendation-Specific Supportive Text
- Several studies evaluating the effect of gamified learning demonstrated an improvement in knowledge acquisition, knowledge retention, and CPR skills.2–5 No studies demonstrated a negative impact on learning or notable adverse effects. The use of leaderboards demonstrated similarly mixed results, with 1 study showing improved CPR performance1 and others demonstrating no significant improvement in frequency of CPR practice of CPR skill.6
- Of the studies that evaluated VR for CPR training, 1 randomized and 1 observational cross-sectional study showed that VR improves knowledge and skills performance in both lay rescuers and healthcare providers.7,8 One randomized study showed no difference compared with ACLS training with feedback in healthcare providers,9 and 1 randomized study found that VR improved bystander response metrics (eg, requesting automated external defibrillator) but decreased chest compression depth, though neither cohort performed chest compression depth within guidelines.10
Synopsis
Learners can maximize their learning opportunities during advanced life support courses by being well prepared before arriving in the classroom.3 Learners can accomplish this by completing precourse learning assignments or reviewing course materials before attending class. Courses providing precourse preparation, such as screen-based simulation,1,2 allow the instructor to focus classroom time on blending newly acquired knowledge with technical skill and teamwork practice necessary to improve learning outcomes. We reviewed the literature to determine if precourse preparation was effective as a supplement to traditional advanced life support training conducted with an instructor.4 Two RCTs addressed the research question; 1 study demonstrated improved performance on some individual CPR performance variables, but neither demonstrated improved overall pass rates.1,2 The literature search identified 3 additional studies in which precourse preparation replaced the first day of a traditional 2-day advanced life support course; these studies were excluded from the current review. Given the unclear benefit and low risk, it may be reasonable to incorporate precourse learning when possible. Future studies should examine the comparative effectiveness of different modes of content delivery in precourse learning.
Recommendation-Specific Supportive Text
- A systematic review identified 2 RCTs relevant to the research question.1,2 In both studies, learners were given access to a computer-based simulation program from 2 to 4 weeks before the start of the course. In 1 RCT, precourse preparation was associated with improved time to defibrillate ventricular fibrillation (112 seconds versus 149.9 seconds; P<0.05) and improved time to pacing of symptomatic bradycardia (95.1 seconds versus 154.9 seconds; P<0.05) but no improvement in course pass rates.1 A second RCT demonstrated no improvement in clinical performance and knowledge with the addition of precourse preparation via screen-based learning.2 It is difficult to fully understand the impact of precourse preparation because both studies provided precourse access for all learners but only 1 trial subjectively monitored whether the learner actually participated in the simulation exercises.2 In that trial, one third of the learners came to class without accessing the precourse simulations. Those learners who did access the simulations spent about 2 hours on average.
| COR | LOE | Recommendation |
|---|---|---|
| 2a | C-LD |
|
Synopsis
According to the Centers for Disease Control and Prevention, opioid overdose deaths in the United States have more than doubled in the past decade, from 18 515 in 2007 to 47 600 in 2017.9 Improving recognition of opioid overdose and increasing lay rescuers’ willingness and ability to administer naloxone has the potential to improve outcomes. A scoping review was conducted to determine the impact of targeted resuscitation and naloxone training on opioid users and lay rescuers likely to encounter an opioid overdose.10 Educational interventions included training programs for family members of opioid users (including naloxone distribution), computer-based training of opioid users, peer-to-peer training (ie, opioid users teaching other opioid users), and brief counseling by emergency department staff.1–8
Educating opioid users5,7 and their friends, families,1 and close contacts5 improves willingness and ability to administer naloxone, risk awareness, overdose knowledge recognition, and attitudes toward calling EMS.3,10 We suggest that people who use opioids or those who may witness an opioid overdose receive training in responding to opioid overdose, including the administration of naloxone. The data reviewed are limited by the inability to link population-level interventions to individual patient outcomes. More research is required to determine which educational interventions provide the greatest benefit by measuring both learner and patient outcomes.
Recommendation-Specific Supportive Text
- Eight studies (1 RCT and 7 observational studies)1–8 assessed the impact of opioid training using a comparator group. These studies evaluated the impact of short educational courses, with opioid users, friends, and family members as participants. Outcomes were heterogenous and included knowledge of risk, identifying overdose, knowledge and skill to respond to overdose, and willingness to aid or phone for help.1,3–8
One RCT found that 60% of witnessed overdoses involving an individual who had been trained within the prior 3 months received first aid and/or naloxone compared with zero in the comparator group.1 In an observational study, 40% of participants who witnessed an overdose in the 12 months after education administered naloxone.5 Another study found that the rate of naloxone administration was higher in those who had received opioid training compared with those who did not (32% versus 0%).4 They found no difference in the rates of calling 9-1-1 or delivering rescue breaths between the 2 groups.4 Another study found no difference in the provision of aid between trained and untrained responders.2 Interventions that included skills practice (ie, naloxone administration) were more likely to lead to improved clinical performance compared with interventions without skills practice.1,11–22
| COR | LOE | Recommendations |
|---|---|---|
| 1 | B-NR |
|
| 1 | B-NR |
|
| 2a | C-LD |
|
Synopsis
Health disparities adversely affect groups that have systematically experienced greater obstacles to health based on social determinants such as race, ethnicity, SES, and gender.25 We defined racial and ethnic populations as individuals and neighborhoods that have historically experienced inequity or prejudice, such as black or Hispanic people and linguistically isolated communities with limited English proficiency. SES was characterized by self-identified income and education by individual or neighborhood. Gender was defined on the individual level as self-identified or clinician-identified male or female gender. We examined whether race, ethnicity, SES, and gender are associated with lower rates of B-CPR or CPR training to understand if targeted training for these populations is warranted.1–24 Predominantly black, Hispanic, and low-SES neighborhoods have lower rates of B-CPR and CPR training.3–5,16 Language barriers are associated with lower rates of CPR training.9,10 Women are less likely to receive B-CPR, which may be because bystanders fear injuring female victims or accusations of inappropriate touching.22,23 The targeting of specific racial, ethnic, and low-SES populations for CPR education and modification of education to address gender differences could eliminate disparities in CPR training and B-CPR and potentially enhance outcomes from cardiac arrest in these populations. Future work examining the racial, socioeconomic, and gender barriers to B-CPR and CPR education is critical to advance our understanding of these important issues.
Recommendation-Specific Supportive Text
- Four retrospective cohort studies and 1 cross-sectional study found that residents of black and Hispanic neighborhoods were less likely to receive B-CPR and that black residents were less likely to be CPR trained.1–5 A descriptive investigation found few high-quality CPR educational resources for Spanish-speaking populations.6 Mixed qualitative studies suggest that language barriers, financial considerations, and lack of information are associated with low rates of B-CPR in linguistically isolated communities.6–10
- Several retrospective cohort studies have demonstrated that low SES is associated with a lower likelihood of receiving B-CPR.11–16 In addition, recent cross-sectional studies found that low SES is associated with a lower likelihood of CPR training.17,18 To address this, retrospective studies have demonstrated the feasibility of using neighborhood mapping to identify low-SES neighborhoods for targeted training.19,20
- A recent study examining gender differences in the delivery of B-CPR found that men were more likely than women to receive B-CPR in public locations.21 Cross-sectional survey studies suggest that layperson responders are fearful of being accused of inappropriate touching, sexual assault, and causing injury to female victims in need of B-CPR.22,23 A randomized simulation study found that subjects were less likely to remove the clothing of a female manikin than a male manikin.24
| COR | LOE | Recommendation |
|---|---|---|
| 2a | C-LD |
|
Synopsis
Appropriate provision of prehospital resuscitative care is an important element in determining outcomes from OHCA.7 Understanding the impact of ongoing exposure (ie, caring for actual patients in cardiac arrest) or general experience (ie, time on the job) on patient outcomes from OHCA may inform staffing and training strategies. A systematic review suggests that EMS provider exposure—both the number of cardiac arrest cases managed over time and the most recent exposure to cardiac arrest (less than 6 months)—is associated with improved return of spontaneous circulation (ROSC)2,3 and survival to hospital discharge.1,8 Results of the individual studies were inconsistent, but those of higher quality that adjusted for known predictors of survival demonstrated improved survival outcomes with higher EMS provider exposure.1 EMS provider experience (years on the job) was not associated with improved survival to discharge.1
It is reasonable for EMS systems to monitor provider exposure to resuscitation to implement strategies to address issues of low exposure or to ensure that treating teams have members with recent exposure to cardiac arrest cases. The benefits of adjusting staffing or supplementing exposure through simulation-based training need to be weighed against the practicality of scheduling and the additional costs of training because they may come at the expense of other potentially beneficial quality improvement activities. We are unable to make any recommendations on the exposure required to care for pediatric cardiac arrest victims.
Recommendation-Specific Supportive Text
- Results of a systematic review identified 2 observational studies that evaluated an impact of provider exposure.1,3 The larger study reporting adjusted outcomes found improved survival to discharge with higher team exposure (number of cardiac arrests in the preceding 3 years). Compared with teams with 6 or fewer exposures, the likelihood of survival was higher in groups with more than 6 to 11 exposures (adjusted odds ratio, 1.26; 95% CI, 1.04–1.54), 11 to 17 exposures (adjusted odds ratio, 1.29; 95% CI, 1.04–1.59), and more than 17 exposures (adjusted odds ratio, 1.50; 95% CI, 1.22–1.86), suggesting a “dose-response” relationship with exposure.1 The remaining observational study reporting unadjusted outcomes found no association between exposure and survival to hospital discharge.
One observational study found lower survival to discharge in patients treated by teams with no exposure in the preceding 6 months compared with those with recent (less than 1 month) exposure (adjusted odds ratio, 0.70; 95% CI, 0.54–0.91).1 Additional studies found no association between team leader cardiac arrest exposure and event survival3 and no association between years of clinical experience of the EMS provider or EMS team and survival to hospital discharge.1,4,9 Two studies reported improved ROSC with higher primary treating paramedic exposure.2,3
| COR | LOE | Recommendation |
|---|---|---|
| 2a | C-LD |
|
Synopsis
Resuscitation councils have offered adult advanced life support courses (eg, ACLS offered by the AHA, Advanced Life Support course offered by the European Resuscitation Council) for more than 3 decades, providing the knowledge and skills required to recognize and treat critically ill adult patients.10 The course is intended for healthcare professionals likely to manage adult patients with cardiac arrest. ACLS course content and instructional design is updated every 5 years to reflect the most current resuscitation guidelines, and recent versions have focused on interprofessional, team-based care via simulation-based training.10–12 A meta-analysis of relevant studies found that resuscitation teams with 1 or more team members having previous participation in an ACLS course results in improved patient outcomes, including ROSC, survival to hospital discharge, and survival to 30 days.9,13 For this reason, we recommend that all healthcare professionals likely to participate in the care of adult cardiac arrest patients take the ACLS course or equivalent training.
The benefits of course participation should be weighed against the costs of taking the course, particularly in low-resource settings where taking ACLS may come at the expense of other beneficial interventions. We are unable to make a recommendation for neonatal and pediatric healthcare providers, given the lack of evidence evaluating patient outcomes from PALS and Neonatal Resuscitation Program courses.
Recommendation-Specific Supportive Text
- A recent systematic review found evidence from 6 observational studies3–8 enrolling 1461 patients with higher rates of ROSC for adult in-hospital cardiac arrest cared for by a resuscitation team with at least 1 member completing an accredited ACLS course compared with patients cared for by a team without members with prior ACLS training (odds ratio, 1.64; 95% CI, 1.12–2.41).9 The systematic review found evidence from 7 observational studies1–3,5–8 enrolling 1507 adult in-hospital cardiac arrest patients for improved survival to hospital discharge or survival to 30 days for patients cared for by a team with at least 1 member completing an accredited ACLS course (odds ratio, 2.43; 95% CI, 1.04–5.70).9 Pooled data from 2 observational studies 5,6 enrolling 455 patients showed no significant association between 1-year survival and ACLS training.9
Additional benefits of ACLS training include faster time to ROSC,5 decreased treatment errors (eg, incorrect rhythm assessment),4 and an association between the number of team members trained and higher ROSC.5
No studies report the impact of ACLS training on intact neurological survival or the impact of course components on patient outcomes. Among the studies reviewed, there was a high risk of selection bias due to differences between study populations. Most studies were conducted before 2010 and may not accurately reflect current standards of care and current ACLS course design, which has a greater focus on team based care and simulation-based learning.
| COR | LOE | Recommendations |
|---|---|---|
| 2a | C-LD |
|
| 2b | C-LD | |
| 2b | C-LD |
Synopsis
Prompt delivery of B-CPR doubles a victim’s chance of survival from sudden cardiac arrest, yet fewer than 40% of victims receive B-CPR in many communities.13,14 Given the relatively low B-CPR rate, assessment of the facilitators and barriers to the performance of B-CPR is warranted. Individual-level facilitators that increase willingness to perform B-CPR include previous CPR training, younger age, and family relationship to the cardiac arrest patient.2,12,15,16 Community-level facilitators include Hands-Only CPR training, mass CPR training (ie, training large numbers), and CPR awareness initiatives to increase bystander performance.1–4 Barriers to bystanders’ initiating CPR include individual-level emotional barriers (eg, fear, panic, lack of confidence, concern of injuring the victim),3,8,12 perception of the victim’s physical characteristics (eg, vomit, blood, female gender, perceived futility of the situation, positioning of the patient),2,5,7–11 and community-level low SES and racial composition.16–21 We suggest that bystander willingness to perform CPR be enhanced through mass CPR training, CPR awareness initiatives, and promotion of Hands-Only CPR. We also suggest that layperson CPR training programs address physical and emotional barriers to bystander willingness to perform CPR. These efforts may improve bystanders’ initiation of CPR and provide avenues for future initiatives tailored to address these known barriers.
Recommendation-Specific Supportive Text
- A cohort study demonstrated that bystanders with previous CPR training were 3 times more likely to perform CPR.2 A 40-minute mass, Hands-Only CPR training of more than 5 500 university students was found to promote B-CPR.3 Community-level promotion of Hands-Only CPR training was associated with increased B-CPR and an increased incidence of survival with favorable neurological outcome.1 Communities with a higher proportion of residents identifying as having CPR awareness, prior CPR training, and higher self-efficacy were associated with an increased likelihood of B-CPR.4 Some studies were limited by prior CPR training and ecological community-level measurements.
- Several survey-based studies of bystanders described vomit, alcohol on the victim’s breath, and visible blood as physical barriers to initiating CPR.5,6 Analyses of dispatch-assisted CPR tapes found that inability to move patients to a hard, flat surface was associated with reduced rates of CPR.7,8 Four retrospective cohort studies found that women are less likely to receive B-CPR compared with men.2,9–11
- Observational studies found that panic, lack of confidence, perceptions of futility, and fear of injury were emotional barriers to initiating CPR.6,12 A survey of university students cited burden of responsibility and difficulty in judging a cardiac arrest as additional barriers.3 These studies suggest that tailored CPR training to address these emotional barriers and providing general awareness of these barriers may improve bystander willingness to perform CPR.
Defining the optimal means of delivering resuscitation education requires robustly designed studies that address important knowledge gaps. Resuscitation education research has been hampered by unique limitations compared with clinical resuscitation research. This can be readily appreciated with the predominance of recommendations in this chapter that are classified as weak and are based on levels of evidence classified as low, according to GRADE criteria.1 We believe that this, in part, reflects inherent limitations associated with the use of GRADE for the evaluation of educational research. Many of the studies we reviewed were insufficiently powered, single-center studies, making it difficult to determine the true impact of the intervention of interest. Collaboration in the form of multicenter research studies would help to address this problem.2 Education research networks provide the infrastructure necessary to support mentorship, grant applications, study design and implementation, and knowledge dissemination.2,3 Another overarching issue prevalent among resuscitation education research is outcome selection.4,5 In a manner somewhat different from other scientific areas, direct linkage of provider performance in simulated environments to performance during actual patient care (or patient outcomes) remains relatively elusive. Over the past several years, a handful of studies have successfully linked educational interventions to clinical outcomes after actual patient events,6–10 but most educational studies examine the surrogate outcomes of learner knowledge and skill performance in the simulated setting. Resuscitation researchers should aspire to report clinical outcomes from educational interventions (Table 2). When the selection of patient outcomes is not feasible, we encourage educational researchers to select quantitative measures that have a known association with improved clinical outcomes from cardiac arrest (eg, chest compression depth). Doing so will allow researchers to establish causal links among outcomes that are similarly reported in simulation-based and clinical studies.11
Our review of the literature identified significant heterogeneity in intervention type and outcome measure type, making it difficult to conduct meta-analyses for many of the key topics. Even for outcomes common across many studies (eg, CPR depth), there was variability in the outcome measure type (eg, mean CPR depth versus percentage compliance with CPR depth per 30-second epoch versus percentage compliance with CPR depth per event). The establishment of standardized reporting guidelines for outcomes from resuscitation education research would address this issue and enable meta-analysis of key questions in the future (Table 2). Acknowledging these shortcomings, it remains true that educational research, like other areas of resuscitation science, has gaps in essential knowledge that require further investigation.
Several general questions bear mentioning as essential considerations for future research in resuscitation education. Because very few studies link educational interventions to patient outcomes, additional research is needed to examine the connections between educational outcomes and survival from cardiac arrest, as well as from other intermediate clinical outcomes known to be contributors to survival (eg, high-quality CPR, time to defibrillation, time to initiation of CPR). Among the studies examining knowledge and skill as outcomes, a disproportionate number examine these outcomes only at a single time point immediately after course conclusion. Future studies should focus on retention of knowledge and skill over longer periods of time rather than exclusively at the end of course delivery, particularly in light of the fact that some teaching strategies may show good short-term improvements but poor long-term learning outcomes. Many of the studies we identified examined certain instructional design features in isolation, or they executed a study design that failed to appropriately isolate the variable of interest. Future studies should be designed to control for potential confounding variables (eg, concurrent educational opportunities, prior experiences, rater blinding) and/or include statistical analyses that adjust for variables of interest. Furthermore, a greater understanding of the combined effect of instructional design features, when applied to specific resuscitation skills, will facilitate improved learning outcomes in the future.
Significant knowledge gaps exist with respect to the economic evaluation of resuscitation education. Economic evaluation is a type of research that examines both the cost and the consequences of at least 2 alternatives (eg, BLS training with and without CPR feedback devices).12 Although current literature has provided evidence supporting the effectiveness of certain instructional design features, educational programs still must balance the potential benefits with costs when deciding whether to adopt a certain method of training. A properly conducted cost-effectiveness analysis can inform these decisions. Future educational research should explore both the effectiveness and the associated costs of training (Table 2). This helps not only to promote the implementation of certain instructional designs but also to establish evidence on how to maximize learning outcomes with limited resources.
| TABLE 2. Overarching Knowledge Gaps in Resuscitation Education |
|
|---|---|
| Topic Area |
Sample Research Question |
| Relevance of outcomes | Is there an association between educational outcomes in training (ie, knowledge and skill), clinical performance, and patient outcomes? |
| Patient outcomes | What is the impact of educational interventions and/or specific instructional design elements on patient outcomes? |
| Standardized reporting | How can outcomes from resuscitation education research be standardized to reduce heterogeneity among studies? |
| Cost-effectiveness | What is the cost-effectiveness of different educational interventions? |
| Optimizing instructional design | How can instructional design features be combined to best optimize learning and patient outcomes? |
| Tailoring instructional design | Which resuscitation skills/competencies are best suited for each instructional design feature? |
| Learning curves and skill retention | What are the learning curves for key resuscitation skills, and how can training be structured to optimize long-term retention of skills? |
The writing group identified several key content areas with glaring knowledge gaps. Assessment that drives learning is among the AHA’s core educational concepts, yet there is a relative paucity of research informing the practice of assessment in resuscitation education.5 Research exploring the source (ie, instructor, manikin, device), timing, and structure of feedback is necessary to inform future course design. A growing number of instruments for formative and summative assessment of learners in resuscitation courses exist in published literature.4 Assessment of healthcare providers spans the domains of clinical knowledge, technical skills, and teamwork. Selecting the appropriate instrument for specific domains should be part of the assessment strategy for training programs. Instruments designed for these purposes should be rigorously tested for reliability and generalizability. Future research would benefit from a description of rater training strategies and greater standardization of use of these instruments across different learner groups and settings (Table 3).
Faculty development opportunities for resuscitation educators ensures that resuscitation training programs are delivered effectively. Although existing literature describes key features of effective faculty development in medical education,13 there is a lack of research as it applies to the training of resuscitation educators. Finally, topics such as the use of cognitive aids during training, hybrid course design (eg, with eLearning and/or other features), artificial intelligence, and augmented reality are of interest but require a greater body of evidence before recommendations to inform future practice can be made (Table 3).
While these guidelines covered some newer educational strategies, such as VR and gamified learning, we also continue to focus on basic constructs, such as spaced learning, booster training, deliberate practice, and feedback. In all of these areas, important knowledge gaps—and thereby opportunities for future study—remain (Table 3) Resuscitation education. With appropriate funding, researchers will be able to explore newer or novel phenomena and also continue to evaluate long-standing paradigms of resuscitation education. With this approach, we will continue to push for enhanced educational efficiency and improved outcomes from cardiac arrest.
| Table 3. Specific Knowledge Gaps in Resuscitation Education by Topic | |
|---|---|
| Topic Area |
Sample Research Question |
| Mastery learning | What are the minimal passing standards for different resuscitation skills, and does incorporation of these standards into a mastery learning model of training improve skill acquisition and retention? |
| Booster training | What are the ideal booster training intervals for key resuscitation skills to prevent skill decay over time? |
| Layperson training | How do we optimize layperson training to improve bystander CPR rates, quality of CPR, and patient outcomes? |
| Teamwork and leadership training | How can resuscitation team structure be modified (eg, inclusion of a CPR coach) to enhance performance, and can training in these new structures improve outcomes? |
| Feedback and debriefing | How does the source, frequency, structure, content, and timing of feedback and debriefing during resuscitation training influence outcomes? |
| Technology in training | How can new and emerging technologies (eg, VR, augmented reality, eye tracking, artificial intelligence) be used to improve resuscitation performance and patient outcomes? |
| Disparities in education | What are the optimal methods to address racial, ethnic, socioeconomic, and gender disparities in resuscitation education? |
| Faculty development | What is the best method of training resuscitation instructors that is both scalable and effective? |
| Assessment of learners | What is the most effective assessment strategy during resuscitation training? |
| Cognitive aids in training | How can cognitive aids be effectively incorporated into resuscitation training programs to support learning? |
CPR indicates cardiopulmonary resuscitation; and VR, virtual reality.
- Adam Cheng, MD, Chair
- David J. Magid, MD, MPH
- Marc Auerbach, MD, MSCE
- Farhan Bhanji, MD, MEd
- Blair L. Bigham, MD, MSc
- Audrey L. Blewer, PhD, MPH
- Katie N. Dainty, MSc, PhD
- Emily Diederich, MD, MS
- Yiqun Lin, MD, MHSc, PhD
- Marion Leary, RN, MSN, MPH
- Melissa Mahgoub, PhD
- Mary E. Mancini, RN, PhD
- Kenneth Navarro, PhD(c)
- Aaron Donoghue, MD, MSCE, Vice Chair
Open table in a new window.
Open table in a new window.
 Login
Login